Science is Now Focusing more on Researching the Placenta
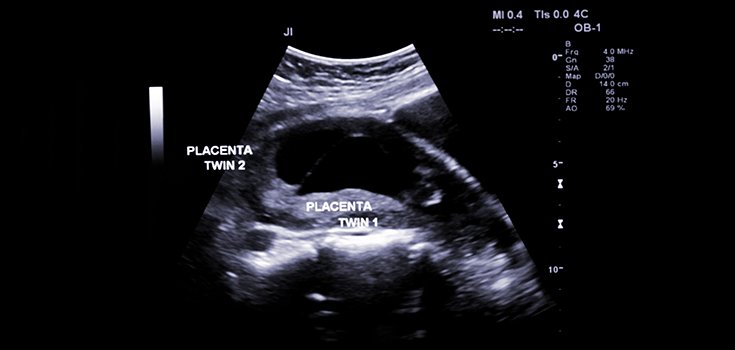
With the threat of the Zika virus passing on life-altering birth defects to children of infected mothers, scientists have taken to studying the human placenta with the National Institutes of Health’s $50 million Human Placenta Project. What is often simply dismissed as “afterbirth” is actually quite helpful in discovering the causes of diseases and other genetic risk factors that can potentially hurt the fetus. [1]
Because the placenta does so much for the fetus, (it acts as its lungs, liver, and kidneys, provides nourishment, and immune defense within the room) it is a wonder that it took so long for scientists to actually take notice of its role in human life and development in a serious way.
“We take it for granted. Yet there are lifelong implications for both the mother and the baby,” stated Dr. Catherine Spong, who is working on the project.
One of the issues that scientists face when attempting to study the placenta is that it is very difficult to monitor as it is growing inside the mother, which is key to the research. Instead, a placenta that is donated has already carried a baby to full-term, and thus finished its maturation.
The Associated Press explains the theories involved in examining a fetus:
“Engineer Avinash Eranki turned over a donated placenta, examining the side that was attached to the mother. That outer layer is made up of cells called trophoblasts that invaded the uterine wall and burrowed into arteries, enlarging them to provide blood flow for the fetus.
The theory: If those cells get off course and the blood vessels don’t widen enough, the downstream effects of a placenta struggling to support the fetus eventually stress the mother’s other organs.” [2]
To combat this, scientists at Children’s National Health System have recreated a 3-D model of the growth of the placenta using a bioprinter. This exciting technology can mimic how the blood supply is created, and the printer actually places human tissue and other things the fetus needs to stay alive.
If successful, the scientists will be able to use the model to detect pre-eclampsia and help the fetus sooner, rather than delivering a premature baby, which is currently the only treatment.
Dr. Anna Penn, a neonatologist at Children’s National, said:
“It’s very exciting to see people focusing on the real-time changes that happen during a pregnancy and how those shape later outcomes. The whole idea is early detection of problems so that if things are going off in the wrong direction, hopefully we can get back on track.”
Sources:
[1] Salon
[2] Japan Times
