Study: Doctors’ Hand Washing Habits Putting Patients at Risk

People take it for granted that doctors and nurses are washing their hands properly before examining them. After all, no one understands germs and sickness like these healthcare professionals do. But a recent study finds that unless doctors are being watched, they tend to neglect proper hygiene.
The study found that healthcare professionals at SCVMC dramatically increased their hand hygiene compliance when they knew they were being evaluated.
For the study, the researchers had two types of auditors assess hand hygiene: Infection Prevention (IP) nurses – considered the hospital’s “hygiene patrol” – and high-school and college-age volunteers who received training on how to perform the exact same assessments, but who were not consistently recognized by hospital staff.
A pattern quickly began to emerge.
Maricris Niles, an infection prevention analyst at SCVMC, told ABC News:
“[We noticed] a very consistent trend that our Infection Prevention nurses were seeing something different than what volunteers were seeing.”
The IP nurses reported much higher compliance rates.
To test whether compliance was being recorded differently by different observers, extra measures were taken to ensure that this was not the case. Ultimately, the difference came down to whether healthcare workers knew they were being watched, which is something they couldn’t always decipher when they were being observed by the students.
Lisa Hansford, one of the recognizable IP nurses at SCVMC, explained:
“When we would come on the floor, I would notice that the nurses or providers were not using the alcohol. Then they would glance up and see me and bend over backwards to lather up.”
The researchers found the hand hygiene rate observed by IP nurses was about 57%, while the young volunteers recorded rates of about 22%. The team at SCVMC was stunned by this gap, and launched a series of interventions to try and increase their compliance rates.
Hand hygiene is a serious issue in hospitals, due to the potential transmission of infections. In 2015, an outbreak of the superbug carbapenem-resistant enterobacteriaceae, or CRE, grabbed national headlines when infections were reported in hospitals and nursing homes in 42 states. CRE are gram-negative bacteria that are moderately to severely resistant to the carbapenem class of antibiotics, considered the ‘drug of last resort’ for such infections. The cases highlighted the problem of a lack of proper sanitation in medical facilities.
Although proper hand hygiene has always been vital in healthcare facilities, the stakes are even higher now that a bacterium resistant to all antibiotics – including last-resort drugs – has been detected in the United States.
A study published in March 2015 found that 1 in 4 elderly patients had drug-resistant bacteria on their hands. It was also expected that seniors in nursing homes and similar care facilities would continue to acquire new superbugs during their stay. [1]
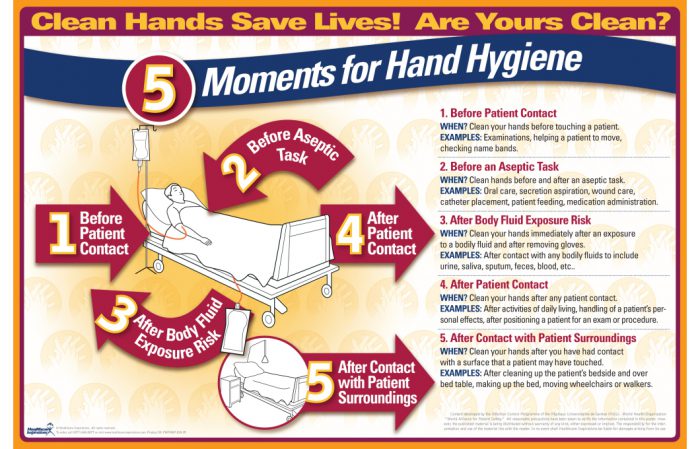
The World Health Organization (WHO) recommends that healthcare providers wash their hands before and after touching a patient or their surroundings, and before any procedure, as well as when they come into contact with any bodily fluids.
A 2002 Centers for Disease Control (CDC) report found that hospital workers washed their hands an average of 5 times per shift and frequently failed to clean the entire surface of their hands. Just 40% of workers were found to adhere to the hygiene recommendations. [2]
Dr. Sharon Wright of the Beth Israel Deaconess Medical Center said that “No measure of hand hygiene is perfect,” noting that, for example, directly observing hand hygiene practices is laborious and could overestimate overall compliance numbers.
The recommendations vary; but generally speaking, doctors and nurses working in ICUs may need to wash their hands more than 100 times during an 8-hour shift. [1]
Researchers from the Santa Clara Valley Medical Center (SCVMC) in San Jose, California, presented their findings at the Annual Conference of the Association for Professionals in Infection Control and Epidemiology (APIC). The conference was held June 11-13, 2016 in Charlotte, North Carolina.
Sources:
[1] Tech Times
[2] Refinery29

Having spent many hours servicing equipment at the facility in question…..3rd world medical graduates bringing their home country values to the USA even when their degree was issued in the USA