Doctors in Australia Ordered to Prescribe Fewer Antidepressants

Australian health experts are warning that antidepressants are not as effective as previously thought. As a result, physicians in that nation are being told to scale back on prescribing the drugs.
Nearly 1 in 10 Australian adults take antidepressants – that’s 10% of the population – and a growing number of children and teens are being prescribed the psychiatric drugs. But the medications don’t work in many cases. In fact, psychiatrists say there has been a drastic breakdown in research backing antidepressants’ effectiveness.
Christopher Davey, a psychiatrist at Orygen, the National Centre of Excellence in Youth Mental Health, told the Sydney Morning Herald that as experts analyze more and more studies of antidepressants, they are discovering that the drugs have proven to be ineffective in 30-40% of people who use them for the sole purpose of treating depression. They are also stumbling across negative trials that were previously not published.
Davey and his colleague Andrew Chanen said earlier studies reported that antidepressants were more effective due to two reasons: pharmaceutical company involvement, and selective reporting of positive results.
The men write in the report:
“The use of antidepressants has continued to rise despite accumulating evidence that they are not as effective as was previously thought.
“Earlier studies had reported much larger effect sizes for the medications, in part driven by the influences of the pharmaceutical industry on selective publishing of positive results and the substitution of outcome measures to report ambiguous findings as positive. Revelations of these publication strategies have done significant damage to the reputation of the medications and to the pharmaceutical companies who make and market them.”
Read: Anti-Depressants Don’t Work For Mild To Moderate Depression
Also, Davey and Chanen believe, another aspect of these earlier positive studies is that the proportion of patients responding to placebos has risen steadily over the past two decades, which has narrowed the gap between the response to the medication versus a placebo.
This perceived symptom improvement on placebo may be due to larger numbers of people with milder symptoms being admitted into trials. These individuals tend to be more susceptible to the placebo response. It’s also likely there was a greater expectation among these subjects that their depression would improve.
Another possibility is that participants simply get better over time, irrespective of the treatment they receive.
The “why” doesn’t really matter. The worry is that, at this point, prescriptions for antidepressants are being handed out for nearly every little unpleasantry, to people who don’t really need the drugs.
The psychiatrists explained that:
“An unfortunate nexus has developed between the diagnosis of depression of any severity and the reflexive prescriptions of medications as monotherapy.”
They’re not saying that antidepressants are useless; rather, that they still play an important role in the treatment of people with moderate to severe depression. But the drugs should be prescribed as part of an overall treatment plan that includes psychotherapy and lifestyle changes.
Read: Study: 70% Of People On Antidepressants Don’t Have Depression
Davey clarified their recommendations to The Guardian:
“We are not arguing that people should stop taking their medication, or that the medications are being over-prescribed.
“But they are being used too often by themselves without considering other components and we point out that antidepressants are just one treatment among a number. Unfortunately, the debate gets a bit polarized, with people arguing whether for or against medication, but it’s not as simple as that.”
A lot of things can contribute to depression, including unhealthy sleep patterns, poor diet, stress, even other medications. Exercise and meditation – and cannabis – can all improve symptoms.
Davey explained that he doesn’t encourage people already taking antidepressants to stop the meds. That, in fact, can be quite dangerous. He said:
“I want to emphasize … that these studies show that, overall, the antidepressant medications are more effective than placebo.
“So I’d say to people keep going with the medication. But I would also say to them, where they feel like the medication by itself hasn’t been helpful, that they go back to their doctor and ask if they reviewed the medication.
“Also where they haven’t seen a therapist, [they could] see if they can see a therapist.”
One of the first articles I wrote for Natural Society concerned the confusion over the causes of depression, and the damage that antidepressants can do in the brains of people who don’t truly need the drugs.
First, since antidepressants first became “popular” in the 1990s, the public has largely come to believe that depression is caused by a chemical imbalance – mainly a lack of serotonin. The truth is, this may not actually be the case. Antidepressants – when they work – increase serotonin, and that seems to alleviate many of the symptoms of depression.
Scientists now believe depression might be caused by an imbalance of gut microbes, or perhaps a virus or bacteria, with one doctor writing that depression should be classified as an infectious disease. This means that antidepressants treat the symptoms of depression and not the cause. These medications carve new pathways in the brain, and may actually be causing brain damage, rather than healing the brain.
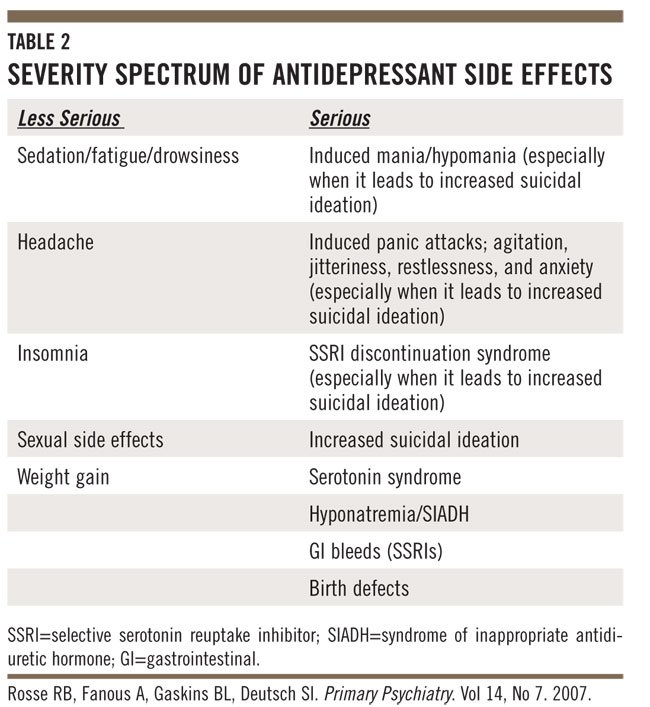
Antidepressant drugs are especially dangerous for children and teens, whose brains are still developing. A review of 70 trials of the most common antidepressants released in March 2016 shows that SSRI (selective serotonin reuptake inhibitor) drugs double the risk of suicide and aggressive behavior in teens under 18 years of age. The link between antidepressants and suicide/aggression have been known for some time, but the review revealed that pharmaceutical companies are still covering up these statistics at an alarming rate.
Last fall, a study found that after taking the drug Paxil (paroxetine), many of the adolescents researchers surveyed reported feeling more distressed, and a shocking number of them attempted suicide. The study also revealed that the FDA approved the drug for use in teens, even though the first trial of Paxil, which began in the late 1990s, found that students taking the medication showed no improvement in their symptoms when compared with two other groups on a main depression questionnaire. (They did rate higher on other, “secondary” measures, such as another scale of mood problems.)
Also, in early 2015, it came to light that less than 1/2 of a sample of psychology papers actually contained legitimate data. Many studies have been retracted, as a result.
Sources:
